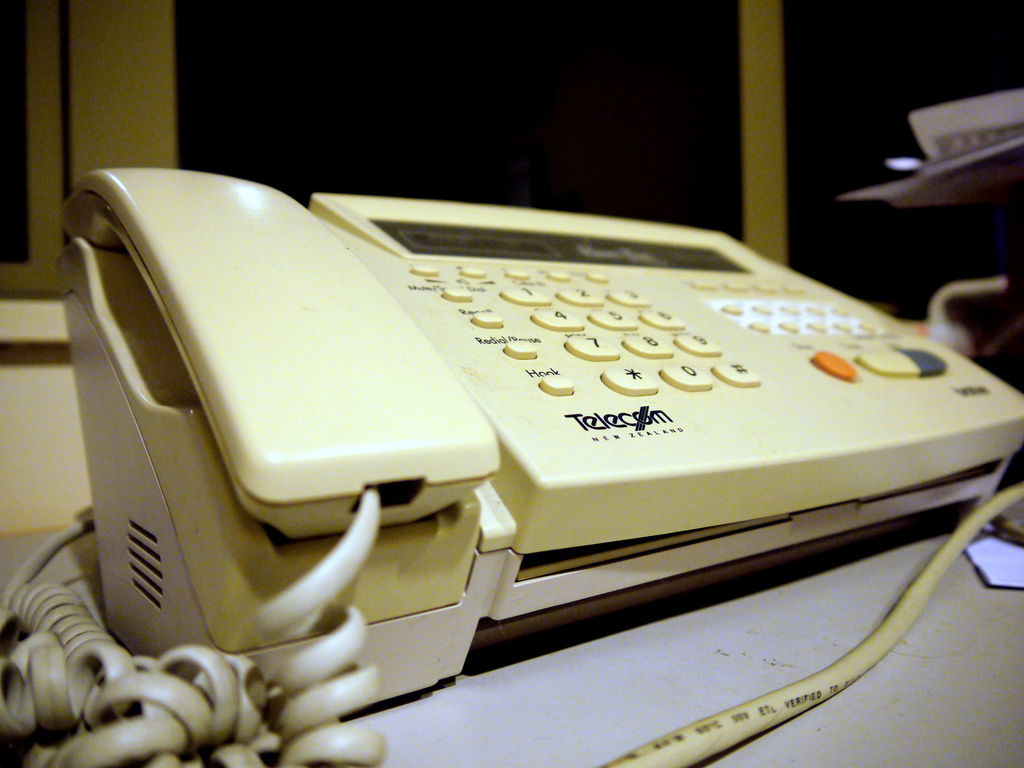
A few minutes into her address at the ONC Interoperability Forum in Washington on August 6, CMS Administrator Seema Verma let fly with an imposing order. “If I could challenge the developers in this room here today to achieve one mission, it would be this: Help us make every doctor’s office in America a fax-free zone by 2020,” Verma said.
That’s going to be a major test of innovation, diligence, and persistence. A 2017 poll conducted by IT website Spiceworks showed 89 percent of small- to medium-sized businesses still using some form of the fax. Further, separate research from International Data Corporation (IDC) found fax usage actually increased year-over-year for 82 percent of survey respondents. In the healthcare sector, fax usage expanded by 9 percent in 2017, IDC reported.
IDC’s study stated, “[Fax] remains a vital communication tool, is relied upon by businesses of all sizes and in all industries, and has an important role within organizations as they embrace digital transformation.” Significantly, such transformation will create value and competitive advantages for organizations that deploy cloud, mobility, data analytics and social technologies in evolving fax solutions.
So, it seems Verma’s directive wouldn’t literally eradicate fax technology from medical offices over the next few years. Instead, IDC predicts an increased presence of software- and cloud-based fax technology that can be integrated with enterprise applications through “secure, trackable and auditable information exchange.” The report adds, “Today’s digital fax server-based systems and cloud services eliminate the standalone fax machines of old and enable integration with users’ desktops, email, back-end applications, and multifunction peripherals.”
Perhaps most promising in IDC’s outlook: About 90 percent of fax users have already integrated or are evaluating the integration of fax with other technologies or applications.
Future of Fax
Faxing, in one form or another, will continue to be used by healthcare providers for years to come, according to Jonathan Coopersmith, the technology historian at Texas A&M University. Part of the support comes from doctors and hospital administrators who believe faxing is more secure than emailing for transmitting protected health information under HIPAA regulations.
At the same time, new generations of electronic faxes have become easier to use. “Faxing is a network technology,” Coopersmith points out. “The more people who use it, the more valuable it becomes.” Future iterations will likely incorporate electronic fax-like capabilities with smartphones, which would make the technology more readily accessible for on-the-go doctors and other caregivers.
And although physical fax machines retain a place in most U.S. emergency rooms, the devices will eventually be phased out, says Peter Alperin, MD, an internist and vice president of connectivity solutions at medical networking company Doximity. “Whether that’s a steep slope or a gradual one is hard to tell,” he comments.
Looking forward, as the design of electronic health record systems improves, data transfer should become increasingly simplified as a matter of course. For example, the 21st Century Cures Act requires EHR systems to exchange data in a way that requires “no special effort.” While that language has yet to be fully parsed, it provides guidance for a more integrated approach to what was formerly known as faxing.
NetDirector supports this vision now. The company’s integration options for healthcare make a digital paperless system much more complete and cost-efficient, from billing to record keeping to lab and imaging work.
To learn more about NetDirector’s cloud-based HealthData Exchange platform, please contact us or request a free demo.