Interoperability Captures Spotlight at HIMSS19
HIMSS19, health IT’s most expansive conference, kicked off on Feb. 11 with the release of a new Centers for Medicare and Medicaid Services (CMS) proposed policy rule detailing the agency’s vision for advancing industry-wide interoperability and patient access to health information.
“We believe patients should have the ability to move from health plan to health plan, provider to provider, and have both their clinical and administrative information travel with them throughout their journey,” according to the rule’s statement of purpose.
CMS Administrator Seema Verma’s public comments during the meeting added depth and clarity: “We are promoting scalable data sharing, not just an individual patient record from hospital-to-hospital, but a model that supports the flow of information across the entire healthcare system. We encourage industry to align in this direction because this is the future.”
Practical Application
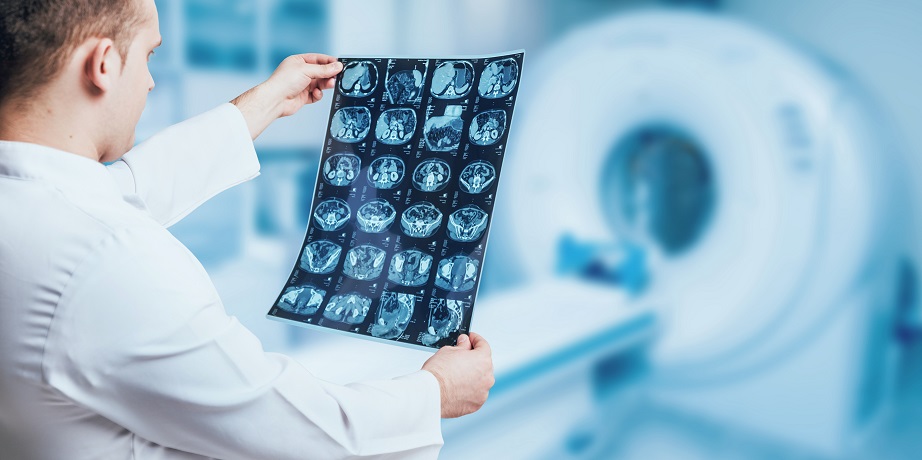
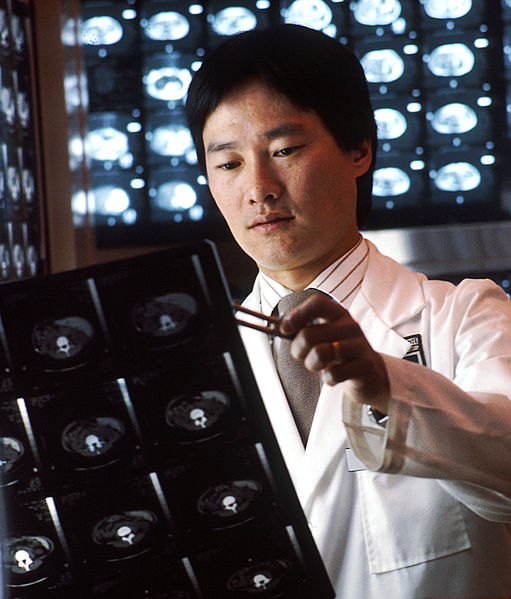
The CMS proposed rule would give patients access to their health information electronically through an application programming interface (API). At the same time, providers could obtain their patients’ health information, regardless of previous sites of care. On the flip side, providers would not be able to restrict information flow to other providers and payers. Additionally, CMS expects payers and third parties to develop software that would ensure seamless data availability when patients change providers, health plans or issuers.
The rule’s timeline is aggressive. CMS stipulated that Medicaid, the Children’s Health Insurance Program, Medicare Advantage plans and Qualified Health Plans in federally facilitated insurance exchanges must be equipped to give enrollees immediate electronic access to claims and other health information by 2020.
Concurrent with the CMS rulemaking, the Office of the National Coordinator for Health Information Technology (ONC), which guides national efforts on health IT implementation/ usage and electronic information exchange, unveiled its own rule on data blocking. The ONC rule implements provisions spelled out by law in the 21st Century Cures Act, which Congress passed in 2016. The rule also provides exceptions to the law’s definition of information blocking. Aside from potential fines (up to $1 million per instance) applicable to health information exchanges, providers or hospitals that block information would be publicly named by CMS.
ONC National Coordinator Donald Rucker, MD, a closing speaker at HIMSS19, told attendees that, in the final analysis, patients should be empowered to access their health data “through a [smartphone] app of their choice, at no additional cost.” Rucker added, “Patients should be able to attach their smartphone to the provider’s endpoint and get their medical data … That’s what modern technology allows.”
Open APIs required for deployment of data sharing under the proposed rules would be based on HL7’s FHIR standard.
Additional Considerations
While early reaction to the CMS/ONC rulemaking has been mostly positive, the American Hospital Association (AHA) opposes a requirement that providers electronically notify other providers when a patient is discharged or moved to another hospital. “We cannot support including electronic event notification as a condition for participation for Medicare and Medicaid,” according to a prepared AHA statement. “We believe that CMS already has better levers to ensure the exchange of appropriate health information for patients. We recommend the agency focus on building this exchange infrastructure rather than layering additional requirements on hospitals,” the statement concluded.
Privacy and security considerations should also be factored into the mix during the 60-day public-comment period for the CMS and ONC rules. Cybersecurity executive Mac McMillan noted, “[The agencies] said, ‘We want you to be more open, but you still have to protect the data.’ Typically, those two things don’t go hand-in-hand … Folks are going to be very concerned they are on the hook for any downstream incidents that occur as a result of openness they have with third-party developers.”
Ahead of the Curve
NetDirector’s HealthData Exchange platform aligns well with the regulatory landscape inherent in the CMS and ONC rulemaking. In short, interoperability’s focus should be on the patient.
HealthData Exchange allows providers and vendors to electronically move clinical and financial data among disparate information systems while adhering to HIPAA and HL7 compliance standards. Less time spent on technology and inputting data frees up providers to deliver an improved patient experience by integrating information flow throughout the continuum of care.
To learn more about NetDirector’s HealthData Exchange platform, please contact us or request a free demo.